CORIX PRO 70 - WM (WALL MOUNT)
When
turning on the equipment, the display will show the screen presented in Fig. 1.
This screen shows the Equipment Model and the software version. At this point,
the equipment will execute a “self testing procedure” in order to early
detect
some kind of mal-functioning. This testing will take a few seconds.
Next,
the display will show the screen presented in Fig. 2. At this point, if the
“F1” key is depressed within 5 seconds, the “Menu” routine will be accessed. If
not, the “Main” screen will be accessed.
When the
“Main” screen is accessed, the display will show the screen presented in Fig.
3.
Once the
“Main” screen is accessed, it is possible to set pre-programmed times for
automatic exposures or set the timer in manual mode. Of course, it is possible at
any time to switch between automatic and manual time exposures.
ERROR AND FUNTIONAL MESSAGES
The Control Panel is provided with a self diagnostic function
which constantly monitors the system and its most important safety circuits.
When a problem occurs, the system will show a message on the display to alert
the user of this
situation. The control unit is constantly
monitoring the Main Line Voltage. If the line voltage is lower than 10% of the
nominal line voltage, the display will show the message presented in the
Fig.21. If the line voltage is higher than 10% of the nominal line voltage, the
display will show the message presented in Fig. 22. Once the line voltage returns to its
operating range, the control unit automatically resumes its operation and the
display will show the screen presented.
CHECKS AND CORRECTION OF POSSIBLE FAULTS IN DENTAL RADIOGRAPHS
LOGIC BOARD ADJUSTMENTS AND SETTINGS
Nominal Operating Line Voltage Setting
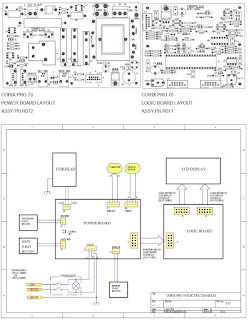
This setting is controlled by the Dip Switch “SWI” (see Fig. 2)
according to the next table. The Dip Switch
is preset in the Factory and must never be changed by the user.
b)
Internal Voltmeter Calibration
This
adjustment is controlled by the Trimmer “POT1” (see Fig. 2) It is preset in the
Factory and must never be changed by the user.
c) LCD
Display Contrast Adjustment.
This
adjustment is controlled by the Trimmer “POT2” (see Fig. 2) It is preset in the
Factory and if necessary, it may be changed by the user.
PRE-SET EXPOSURE TIMES
The following tables of pre-set exposure times in seconds show the
rated exposure time for a nominal line voltage of 120Vac (230Vac) and the final
corrected exposure time, as a function of the line voltage correction factor, patient
size and type of Film (D, F or Digital Sensor) for the minimum 108Vac (207Vac)
and maximum 132Vac (253Vac) line voltage operating range.
PRACTICAL PROCEDURES FOR MEASURING TECHNICAL FACTORS
KVp is defined as the high voltage value applied to the X-Ray tube
after preheating time. KVp value should be measured by a non invasive
instrument with an accuracy of over 2% to the nominal value.
The anodic current value (mA) is
defined as the average value of a steady state current through the X-Ray tube
after pre-heating time.
The anodic current value should be measured using a digital voltmeter. To do this,
it is necessary to remove the Tube head plastic covers. This operation must be
performed only by a qualified technician. To take this measurement, the digital
voltmeter should be selected on DC and read the voltage drop at the ends of a 1KΩ,
1%, assembled on the Tube head. The relation of transformation is given by 1mA
= 1V. Execute an exposure of at least 1s.
The time interval measured from the moment where the anodic peak current first exceeds
25% of the steady state to the moment it again reaches 25% when decreases is
called the exposure time (t).
When taking a measurement of this time, nominal line voltage should be selected,
and a digital memory oscilloscope should be used to read the voltage drop
across the 1KΩ resistor. The
“pre-heating time” is the time taken for the anodic current to reach 25% of its
steady state value.
MEASURING EXPOSURE TIMES
The use of non-invasive equipment, when measuring functional
parameters of XRay devices like exposure time, has led to introduce some
interpretation issues.
The root of these issues is due to the anodic current wave form which is represented
in the next figure: IEC 60601-2-7
(1998) regulations reads: “in equipment where the filament is switched on and
high voltage is applied simultaneously, the exposure time is calculated as the
interval between the instant when the anodic current exceeds 25% of the nominal
value and the instant when it goes below such value”. The last figure shows the
anodic current wave form for an exposure of 0.2s with a pre-heating time of
0.23s. It can be seen that the time named “Delta” measured in the interval when
the anodic current exceeds 25%, represents the actual exposure time (204.0ms).
Although,
non-invasive methods can be simpler to perform than the invasive methods, they
may lead to errors which can be considerable when determining exposure time.
Calculations of exposure time obtained by using non-invasive
methods
may lead to the conclusion that the unit timer is not accurate enough to meet
the regulations.
Electrical Features
The supply line must meet the requirements specified on Label # 2,
located on the Control Panel:
- 120 VAC +/- 10% – 10 Amp., 50/60 Hz, single-phase mains voltage + ground,
or:
- 230 VAC +/- 10% - 6 Amp., 50/60 Hz, single-phase mains voltage + ground.
The equipment must be wired to an electrical panel whose characteristics comply
with the electrical regulations in the country where it is installed. A
dedicated line protected by a 10A circuit breaker is recommended.